A Lesson Remembered

The expression goes, “lesson learned” (actually so many different variations). If you read my last post, “Raw And Unfiltered,” I am titling this post, “A Lesson Remembered.” The lesson that I remembered was learned long ago, and having two college age daughters, it is a lesson that I have been trying to ingrain in their thought processes, their confidences, their lives, often. I have to modify that “dad talk” a little bit, with just a disclaimer, that sometimes we forget that sage advice.
So what happened two days ago, ended up being the beginning of a very, very bad day. The opposite of King Meidas where everything he touched turned to gold, it appeared my day was turning into one giant pile of poop emoji, getting bigger as the day went by. To be fair, each issue that came up, was bad news, with the potential for one situation turning catastrophic. Everything piled together was like a dormant volcano building up so much pressure inside its dome, bound to erupt as the lava needs to go somewhere, I felt like a volcano. And to no surprise, I did erupt.
Taking a slight step back, when I have my discussions with my daughters, a.k.a life lessons, being in college, pressure is something that they often face, whether it be an exam, project, or group event, and not everything works out perfectly or as expected. We talk about the things we have control over, and the need to let go of what we cannot control. I also tell them about the need to change their thought process and the way to do that is to change the oxygen going to their brain by temporary altering their breathing, staggered, a trick I learned in therapy a long time ago. Closing my eyes, or focusing on a particular object, breathing in through the nose slowly for a count of four, then with lips pressed, breath out through the mouth slowly for a count of five. I repeat this three or four times, more if necessary, until I get my thoughts to slow down. Once that happens, I can think clearly again, and deal with the subject at hand.
But Wednesday was different. Only having time to look back now, I got that phone call on an empty stomach. I was definitely not expecting that phone call, and definitely did not expect that news. I was completely taken by surprise. Under normal circumstances, I would have handled things much differently than what I wrote last post. I know that as fact. Before I could enact my breathing exercises however, INCOMING!!!!!, I got hit with some more bad news, totally unrelated, and totally unexpected. Having not resolved my earlier problem, now I had a second one to deal with simulaneously, all the while, not changing my thought processes. This was not going well, as my reactions and responses were getting worse, and somewhat aggressive.
And then a third call came, and with the feels of a “sucker punch,” the caller in a calm voice, and kind of confident, like “no big deal,” hit me with an issue that had the potential to turn my life upside down. That was it. The dome had cracked, the volcano was ready to blow. My reactions to that caller, who was just a “messenger” doing their job, were angry, unprofessional, and for his sake, undeserved as he did not create the situation, others in his chain had done so. But I was going to make it clear, that a terminating ending was not an option, and nor were any of the solutions he was reading to me, likely from a prepared manual. Again, I normally think of myself as a calm and rational thinker, but unable to get to that status from the first call that came that day, I was in a position I did not recognize, nor did it feel good. Remember that, “it did not feel good.”
Several hours after that final phone call, my thoughts had stopped spinning like a tornado in my head. I was once again able to think and process, and knocked out one of the issues, actually the second in occurance right away. Then I took on the original issue that started it all, and within a half an hour, speaking with someone else, an advocate of mine, that issue got taken care of. Finally, the biggest problem of all was all that was left, but only that to deal with. I began to put together a strategy to fix what this particular company had done to me, and was unwilling to make right on their end. At the end of the day, neither of us stood tall and victorious, they did not get their way, and I was not given any relief, but using the control that was put back into my hands, and my managed thoughts, I came up with a different solution, not perfect, but will put things back in balance.
Phew!
Wednesday took a physical toll on me, one that I had not felt in a long time, and honestly, that long time was not a good time either, in fact, it almost killed me. Just like in 2008 with my heart blockage, I had put my body, and my heart, under so much stress two days ago because of my reaction. But wait, it wasn’t my fault, those behind the phone calls caused the stress. Sure, but I know that I do a much better job of controlling my reactions, which is something I constantly counsel my daughters when they come to me, feeling pressures at school.
Adulting my daughters is a whole different stage of parenting than Barbies and school stuff. The pressure, a good pressure, to make sure that I teach them as much as I can how to handle life, how to handle situations that get thrown at them as adults like I had to deal with, continuing to build their confidence, and a whole lot of personal management skills such as: communication, controlling emotions (duh), problem solving, time management (which proudly they do very well), understanding money and decision making. And then there is the personal stuff: self-respect, empathy, self-care, and so much more.
Honestly, these are all things that I wish had been taught to me, but weren’t. So I was and still am winging it. But from the results they are experiencing, while I can take credit for giving them that direction, their results are all their own.
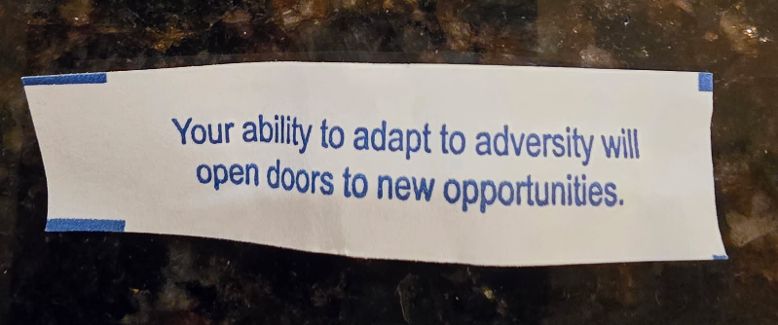
I had Chinese takeout for dinner on Wednesday, and this was my fortune inside my cookie. Too bad I didn’t have it on Tuesday, the heads up would have been appreciated, and much less stressful. When it comes to my daughters, I do try to lead by example, if I am going to talk the talk, I walk the walk. And I have shared this mistep with them, as well as how it made me feel physically afterward, and importantly, not to allow myself to respond that way again. I can get the things done I need, or maybe sometimes I cannot. But the physical stress on the body and mind is a game-ender. I just needed that reminder.


